Osteoarthritis
Crackling, stiff, and swollen joints may be a sign of a day of unusually vigorous activity, but if these symptoms persist for a longer period of time, they might point to something more. Osteoarthritis is a chronic condition that you can manage with minimal intervention if diagnosed in its early stages. Here’s what you should know about this common condition that often leads to painful joints.
What is osteoarthritis?
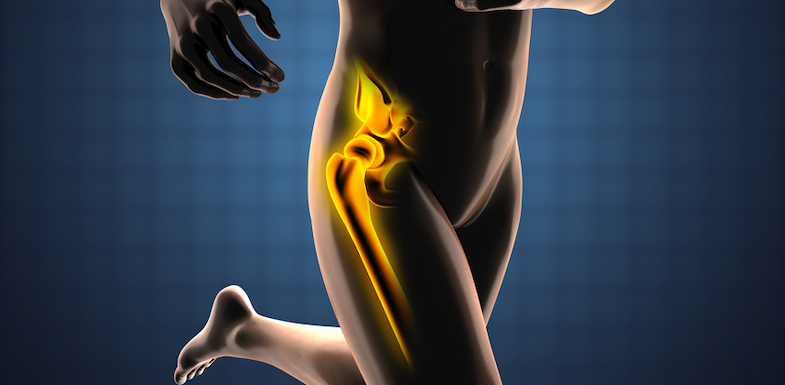
Osteoarthritis (OA) is a type of arthritis characterized by a loss of cartilage and the formation of bone spurs in joint spaces. The anatomy of your joints offers insight into how this condition develops.
The end of each bone, where it contacts another bone, is coated with a soft, compressible tissue called cartilage. Cartilage helps your joint glide smoothly, prevents the two bones from rubbing together, and acts as a shock absorber. This cartilage can become damaged, though, as a result of wear and tear over a number of years or because of a specific injury or other condition.
If the damage to the cartilage is bad enough, the two bones can begin to rub together. This leads to significant pain, inflammation, and a loss in flexibility in the joint itself. Additionally, damaged cartilage may break off into the bursa (the sac of synovial fluid found around the joint). This can lead to bursitis (in addition to the osteoarthritis).
The most common joints affected include the hands, knees, hips, and spine.
What causes osteoarthritis?
Although osteoarthritis most frequently affects people over the age 70, the specific cause of cartilage deterioration is not known. It is not just a disease of aging, but rather the result of a combination of factors that include genetics, overall joint degeneration, and other mechanical processes.
Possible risk factors for osteoarthritis include:
- Obesity
- Gender (women are more likely to develop this condition)
- Muscle weakness
- Repetitive use of joints
- Improper use of joints
- Joint trauma
- Joint instability
Osteoarthritis symptoms
Symptoms typically include the following:
- Joint pain with movement (alleviated by rest)
- Limited range of motion
- Joint swelling
- Joint stiffness after periods of inactivity (such as morning pain or pain after sitting for long periods)
This pain usually occurs for minutes after movement but can last hours. As osteoarthritis progresses, pain can occur during rest and at night.
Joints most often affected by osteoarthritis include the:
- Knee
- Hip
- Joints closest to the fingertips
- Thumb
- Spine, both in the neck and lower back area
Diagnosing osteoarthritis
To obtain a diagnosis, your doctor will take a history and perform a comprehensive physical exam, They’ll pay close attention to:
- Joint tenderness
- Any limited range of motion
- Deformity and joint enlargement
- Swelling
- Crackling sounds heard in joints
Once a physical exam indicates osteoarthritis, an X-ray can confirm the diagnosis if it shows narrowed joint spaces, cartilage loss, and spur formation. X-rays can also determine the severity and follow the progression of osteoarthritis over time.
When your doctor suspects that there is an underlying comorbid condition, they may also order lab tests to rule out other potential causes of your symptoms.
7 osteoarthritis treatment approaches
The goal for treating osteoarthritis is to control your pain and minimize disability through a wide spectrum of treatment options. These treatments range from simple changes in your lifestyle to more interventional approaches that can include surgery.
Here are seven osteoarthritis treatments that might work for your pain and other symptoms.
1. Exercise
People suffering from this condition may think that resting the painful joint is the best option, but movement is actually often better than rest.
Exercising safely with osteoarthritis keeps joints lubricated and maintains (or restores) range of motion. For example, low-impact exercise like walking and swimming can be very helpful in slowing the progression of their symptoms.
2. Rest
In the acute phases, your doctor may advise rest, but don’t overdo it. Too much rest can cause joints to become restricted.
See our notes on exercise, talk to your doctor, and start moving safely when you can.
3. Losing weight
Losing weight minimizes stress on the joints.
Luckily, an increase in exercise (beneficial for osteoarthritis) can help kickstart a weight loss program or help you maintain a healthy BMI.
4. Physical therapy
A physical therapist can design specific exercises to keep your joints mobile and restore range of motion.
5. Over-the-counter and prescription medications
In the early stages of osteoarthritis, you can alleviate acute flare-ups of pain with over-the-counter analgesics, such as acetaminophen, and non-steroidal anti-inflammatory drugs like ibuprofen.
Additionally, for severe cases of pain and inflammation, anti-inflammatory medications can be prescribed. Generally, opioid medications are not recommended for the management of any chronic pain condition (except in severe acute phases).
6. Joint injections
For certain joints, steroid and hyaluronic acid injections may also provide short-term control of pain. These injections control inflammation and pain with a combination of anesthetics and steroids.
Often, joint injections can allow you to manage short-term pain flare-ups while you undergo exercise or physical therapy to treat the underlying cause of your pain. Learn more about this approach in the following video.
7. Surgical intervention
If osteoarthritis progresses to the point where surgical intervention is necessary because more conservative treatments have failed, joint replacement, arthroscopy, or an osteotomy (bone is removed from the joint) may be beneficial.
Surgery does come with risks, but a specially trained pain management specialist can discuss all of your options and help you weigh the benefits and risks.