Back pain affects approximately 80% of people at some point in their lives, with lower back pain being the most common complaint. Although minor aches and pain or an acute injury may disappear on their own with rest and gentle stretching, some conditions require more attention and time, especially if the pain becomes chronic. One of these conditions is herniated disc. Knowing what to do for herniated disc often depends on when you begin your treatment. Here are 14 approaches that may help you.
What is a herniated disc?
A herniated disc occurs due to the spinal column’s unique combination of strength and weakness. The spine is made up of 33 vertebrae in five different sections:
- Cervical (neck)
- Thoracic (upper back)
- Lumbar (lower back)
- Sacrum (bottom of the spine)
- Coccyx (largely immobile bottom tip of the spine)
These vertebrae are held in place with connective tissue and ligaments to protect the spinal cord and nerves that emerge from the spinal column. Facet joints help further stabilize this structure.
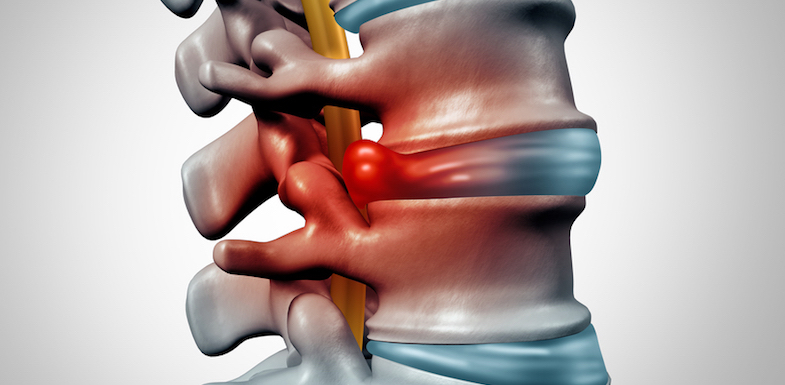
Between each vertebra is an intervertebral disc. These discs are small sacs of jelly-like fluid called nucleus pulposus. Intervertebral discs provide a cushion between vertebrae, a sort of shock absorber in the spine that allows for smooth, comfortable movement along the spine.
A herniated disc occurs when pressure or force exerted on the spine causes the intervertebral disc to push between the vertebrae and rupture, releasing some or all of the nucleus pulposus.
Herniated disc vs. bulging disc
Herniated disc differs from a bulging disc in that a bulging disc is still intact, just protruding from between the vertebrae.
A herniated disc has actually burst and no longer provides any cushion or shock absorption. Bone begins to rub painfully on bone, leading to symptoms that may be unrelieved by most comfort measures.
What causes a herniated disc?
Common herniated disc causes include:
- Disc degeneration: The natural process of aging causes wear on a disc, making it susceptible to herniation
- Spinal stenosis: This narrowing of the spinal cord is also most often seen in older people
- Injury: Trauma to the spine can cause disc herniation
- Repetitive motion: People who work jobs with repetitive motion and heavy lifting are more likely to suffer back problems (including herniated discs)
Genetics also play a part in the development of herniated discs, as does a person’s weight and occupation. More weight on the body tends to mean less activity and more stress on all of the body’s structures. Physically demanding occupations or those with repetitive motions also put workers at increased risk of a herniated disc.
Do I have a herniated disc?
Herniated disc symptoms are difficult to ignore. In addition to pain that can be regular or intermittent, other herniated disc symptoms can include:
- Leg pain: Herniated discs can lead to sciatic pain, a pain that radiates from the lower back, across the buttocks, and down the side of your hip and leg. This pain may be shooting with sudden movement (i.e., when you sneeze) or it may be a dull, constant ache that worsens with too much standing or sitting.
- Numbness and tingling: These symptoms are a sign that nerves are being impinged or compressed by the vertebrae.
- Weakness: Weakness develops as nerve involvement continues.
If the herniated disc is in your neck, you may experience pain across the shoulders and upper back. This may worsen as the nerves continue to compress.
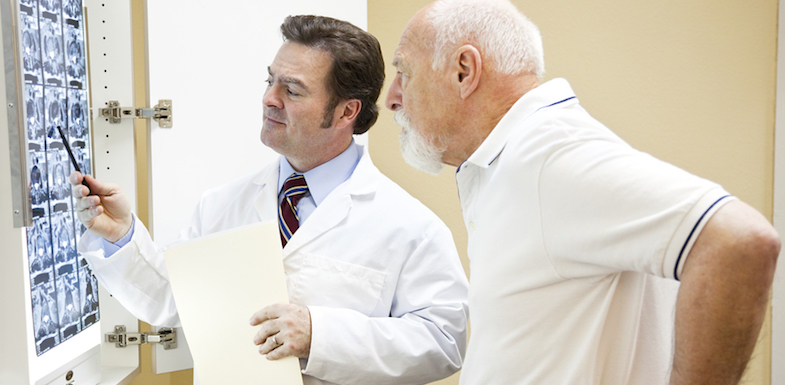
In some instances, people with herniated discs have no symptoms. The only way to confirm a diagnosis is to visit your doctor. They will conduct a thorough physical exam that might include a CT scan, MRI, or X-ray (to rule out other conditions). Your doctor will also test your strength and reflexes, but imaging is the best way to get an accurate diagnosis.
It is important to get a proper diagnosis not only for the herniated disc but also the underlying cause. Your treatment approach may vary depending on what caused the disc to herniate. If the disc is herniated and treated but the underlying cause remains, re-herniation is possible.
What to do for herniated disc: 14 approaches
For some people, a herniated disc resolves itself without any intervention whatsoever. The symptoms may be minimal and simply disappear on their own.
For others, there are a variety of herniated disc approaches to ease symptoms and prevent further injury. Here are 14 approaches to treating herniated discs, from steps to take when you first notice pain to more interventional treatment options.
Note though that of the most serious herniated disc symptoms is a sudden loss of bowel or bladder control. This may be accompanied by suddenly worsening symptoms or something called saddle anesthesia (numbness in the areas that would touch a saddle – back of the legs and inner thighs). If this occurs, treat it as an emergency situation and head to the ER immediately.
First steps
When you first notice herniated disc pain, there are steps you can take to ease symptoms, even before a diagnosis.
1. Brief rest
Although rest is not indicated as a long-term strategy for the treatment of herniated disc, in the acute phase it can be necessary.
Most pain physicians do not recommend rest for longer than three days, but it can be very healing and helpful when the pain is at its peak.
2. Hot and cold therapy
Treating back pain with hot and cold therapy can work well when combined with rest.
Hot therapy (i.e., with a heating pad) can relax and loosen muscle spasms, while cold therapy (ice packs and frozen peas, most often) reduce inflammation and can ease pain.
3. Over-the-counter medications
Some pain and inflammation can be easily managed with over-the-counter pain medications like ibuprofen and naproxen sodium.
These should only be taken as directed by your doctor, as they can come with a host of gastrointestinal side effects when taken in large quantities over a long period of time.
4. Exercise
Disc degeneration may be a natural occurrence as we age, but you can support a strong, healthy back with regular exercise. In addition to whole-body exercise like walking, running, swimming, and biking, targeted exercises for a strong core and back help support the structures of the spine and reduce the chances of injury and pain as you age.
These approaches work best for mild pain in the beginning stages of disc herniation. It may be possible to slow, halt, or reverse the progression without further treatment, as discussed below.
Advanced care
If you find that your pain persists after non-interventional approaches, it’s time to talk to your doctor and explore other options.
1. Physical therapy
Physical therapists work with your pain specialist to design an exercise program for your herniated disc.
They will work with you on the proper form and technique to maximize your workout for best results. Most programs combine stretching routines with targeted strengthening exercises.
2. TENS unit therapy
Transcutaneous electrical nerve stimulation (TENS) replaces pain signals with a mild buzzing sensation.
A mild electrical pulse is delivered through the skin to the nerves as close to the area of pain as possible. The patient controls the signal with a small, cellphone-sized power pack. The electrical signal disrupts pain signals and can offer significant pain relief. Many patients find that a TENS unit relieves pain when other options do not.
3. Radiofrequency ablation
Radiofrequency ablation uses heat to destroy pain-sensing nerves and disrupt the pain signal caused by a herniated disc.
This procedure may offer long-lasting pain relief, but some patients may need more than one treatment.
4. Steroid injections
Steroid injections can help with herniated discs in both the lumbar and cervical spine.
Some patients find that the risks of these injections are worth the opportunity to avoid more invasive surgeries for their herniated disc.
5. Percutaneous discectomy
Herniated disc surgery is a treatment of last resort after other conservative approaches have failed.
A percutaneous discectomy removes the disc material to relieve pressure on the nerves. This procedure is considered less invasive than other types of surgery, some of which may fuse vertebrae together for support or insert pins to maintain space between the vertebrae.
How to heal a herniated disc naturally
As stated above, many people with herniated discs do not require any medical intervention beyond their diagnosis. There are steps you can take at home to start on the path towards herniated disc recovery.
1. At-home care
At-home care for herniated disc means using your body mindfully as you go about your daily tasks. Pay attention to the ways you reach for things on shelves or how you bend over to tie your shoes. Are you engaging your core as you move? Are you picking up objects the correct way? This can help support your healing back.
Likewise, at-home care means taking care of yourself with a proper diet. Look for anti-inflammatory foods that include plenty of fresh vegetables and fruit, lean proteins, and whole grains. Not only will this give your body the fuel it needs for healing, but it might also help you gain (or maintain) a healthy BMI.
2. Massage
Massage can help soothe tight muscles and areas around the herniated disc but don’t use it for the area of the disc itself, especially in the acute phases.
After the acute phase passes, massage can help you reduce stress and tension in the back. Work with a therapist who has extensive experience with sports massages or care for those with back conditions.
3. Herniated disc exercises (plus herniated disc exercises to avoid)
The best herniated disc exercises are those that help you stabilize your core, bringing length to your spine, and building muscles on the lower back, belly, and sides of the abdomen. Think side planks, bridge poses, and partial crunches.
Additionally, tight hamstrings can make your herniated disc pain worse. A simple L-shaped fold at the wall and hamstring stretches on the floor (use a belt or a scarf for support, see below) can help loosen tight hamstrings and give you more freedom in your spine.
There are also exercises to avoid when it comes to herniated discs. Although stretching out your lower back in a deep forward bend may feel good (and seem like it’s helping stretch your hamstrings), you may reach a point where the stretch gets painful. Too much stretch in that area, or too deeply stretching when your body isn’t ready, can make the pain worse.
4. Yoga for herniated discs
Yoga for herniated discs is one of the best things you can do for your body and mind. Find a therapeutic yoga class near you, and get there early to talk to the teacher so they know you are working with a healing back.
Focusing not only on a sequence of breath-supported, low-impact exercise but also on training your mind to remain in the moment without judgement can help you manage your pain as your back heals.
5. Back brace for herniated disc
One of the best treatments for lower back pain, including pain from a herniated disc, is to get a little support.
Back braces can help you go about your daily life with less pain, especially as you work with your doctor to coordinate other treatments. You can also use them while engaging in low-impact cardio or other exercises.
At Arizona Pain, we know what to do for herniated disc, and it starts with a proper diagnosis and a comprehensive treatment plan to help you get your life back. Get in touch today.