Fibromylagia is a neurological disorder that affects approximately 12 million people in the U.S. This chronic disorder causes aches and pains in the body that are severe enough to impact normal activity and disrupt sleep. A person with fibromyalgia may feel pain in the muscles, tissues, joints, and tendons in different areas of the body. Along with these physical symptoms, people suffering from fibromyalgia also experience mental issues as a result of fibromyalgia, including depression and anxiety. Fibromyalgia can also cause deep fatigue and exhaustion, even with very little activity. Even with so many people suffering from fibromyalgia, it remains a difficult disorder to diagnose. One of the most valuable tools for diagnosis was defining fibromyalgia tender points.
The history of a fibromyalgia diagnosis
Fibromyalgia is a term that has only been used in the last few decades to describe a condition of widespread pain throughout the body that also includes fatigue, poor sleep quality, and mood issues. It is possible, however, that mentions of a fibromyalgia diagnosis date all the way back to the 1600s.
Fibromyalgia has had many names throughout the years including:
- Rheumatism
- Muscular rheumatism
- Fibrositis
Since physicians could not find any evidence of inflammation, these names were replaced with fibromyalgia in 1976. This translates from its Greek roots into “pain in the muscles and tissue.” While a fibromyalgia diagnosis is still difficult to establish today, there have been many recent advances. Research has led to promising tools and guidelines to help pain doctors and patients alike. One of the earliest was the fibromyalgia tender points scale.
Understanding fibromyalgia
Fibromyalgia affects about 4% of the U.S. population (~ ten million people) and is predominately found in women.
Fibromyalgia is not a condition of exclusion, but its symptoms are common in many other illnesses. To make things more complicated, fibro symptoms can appear on their own or in tandem with another disorder. Identifying the cause of each can be problematic. This situation is exacerbated since fibro is a waxing and waning condition, making patterns more difficult to recognize even with thorough tracking.
Although researchers agree that there is a neurological component to the disease, many previously believed that it was all in a person’s head. Some studies have pointed to risk factors such as a genetic predisposition to feeling pain more intensely. Other evidence connects the development of fibromyalgia to a stressful or traumatic event, repetitive injury, or other disease. Sometimes fibromyalgia has no clear cause or trigger and develops on its own.
Women are three times more likely to develop fibromyalgia as men, and people with certain illnesses already present may have an increased risk. Autoimmune disorders such as lupus and rheumatoid or spinal arthritis sufferers develop fibromyalgia at a higher rate than those without these conditions.
There is no simple, scientifically-supported test to identify if someone has fibromyalgia. According to the National Fibromyalgia Association, it takes the average person five years to be diagnosed with fibro and this is generally after extensive other treatments have occurred. Misdiagnosis can still occur, but there are far more developed and data backed approaches that physicians use today.
Fibromyalgia diagnosis – developing the modern view
In 1981, the first clinical study was published that confirmed that symptoms and tender points of fibromyalgia could be found in the body. This study also established the first data-driven criteria for this condition.
In 1990, the American College of Rheumatology (ACR) created the first set of guidelines to help diagnose fibromyalgia. These guidelines set forth the following formal criteria for a fibromyalgia diagnosis in a research context:
- The patient must have a history of widespread pain lasting more than three months
- This pain must affect both sides of the body and be present above and below the waist
- Of the 18 tender points designated on the human body, at least 11 of them must be in pain
Before these guidelines were released, a fibromyalgia diagnosis was completely subjective and many were skeptical that the disorder even existed. Even with these new guidelines, fibromyalgia is a condition that can come and go, so using the fibromyalgia tender points criteria can be misleading or change from day-to-day.
Fibromyalgia tender points
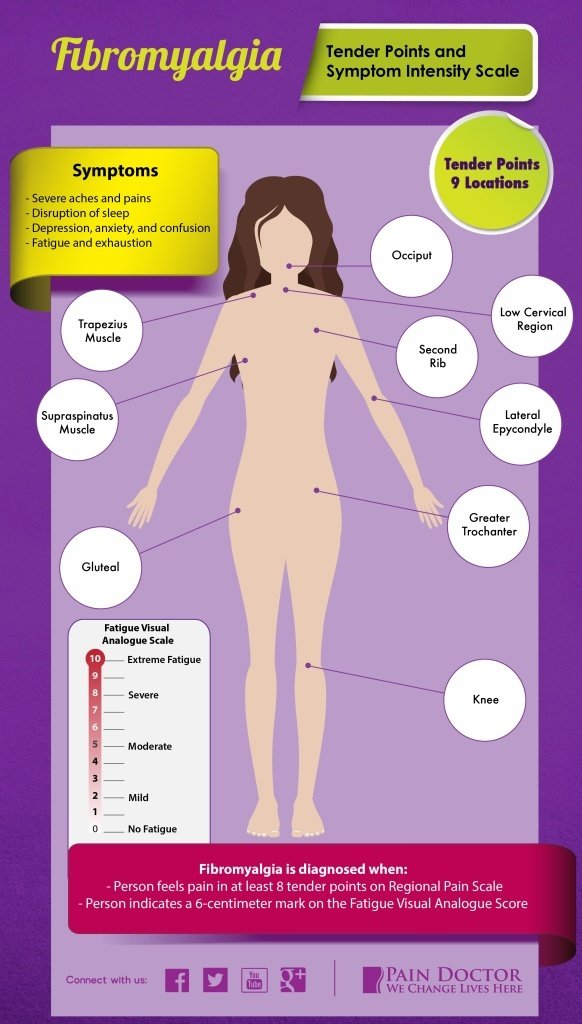
Although most of the population has a spot or two on their body that may be more sensitive than others, people with fibromyalgia often experience excruciating tenderness in very specific locations that are spread across their body. Tenderness is generally mirrored on both sides of the body and is located at nine specific places on the body.
The nine fibromyalgia tender points locations are as follows:
- Low cervical region: Front neck area just below the chin near the C5-C7 vertebrae
- Second rib: Front chest area below the collarbone about 2 inches from the shoulder joint
- Occiput: Back of the neck at the base of the skull
- Trapezius muscle: Back shoulder area where this large muscle drapes over the top of the shoulder
- Supraspinatus muscle: Shoulder blade area just at the top of the shoulder blade
- Lateral epicondyle: Elbow area in the inside of the arm crease
- Gluteal: Rear end at upper outer quadrant of the buttocks
- Greater trochanter: Rear hip in the back
- Knee: Knee area on the inside where the fat pad sits
These nine areas are also sometimes called fibromyalgia tender spots. Because fibromyalgia cannot be diagnosed with a lab test, counting fibromyalgia tender points and taking a detailed patient history were often the best ways to get a clear diagnosis. Scroll to the infographic at the end of this post to see these.
You can also see these in the following video.
The Symptom Intensity Scale
To build on the fibromyalgia tender points scale, the Symptom Intensity Scale was developed using survey results from nearly 12,800 patients with osteoarthritis, rheumatoid arthritis, or fibromyalgia. These patients located pain in 38 anatomic areas of their body and then also completed a fatigue visual analogue scale. The fatigue analog scale requires a patient to mark their level of fatigue on a ten-centimeter line on the day they identified their pain symptoms.
In 2006, Frederick Wolfe and Johannes J. Rasker completed an evaluation of 25,417 patients using the Symptom Intensity Scale and found that it was the best and clearest diagnostic tool for fibromyalgia. They also found that higher Scale scores indicated increases in hospitalization, disability, serious medical issues, and death.
Because of this relationship, the Scale can be used to measure overall health and also predict outcomes for patients with a number of diseases. It uncovers “hidden” illness that accompanies the presenting illness, such as depression or anxiety in a patient with rheumatoid arthritis.
Updated 2010 criteria
While the fibromyalgia tender points are still helpful, they’re not the only path to diagnosis for medical professionals. In 2010, the American College of Rheumatology published another set of criteria for fibromyalgia. It eliminated the fibromyalgia tender points count and replaced it with the widespread pain index (WPI) and symptom severity scale (SS).
The WPI calculates if a person has experienced pain in the last two weeks in 19 separate general body areas. Each body area is assigned a one if there is pain or a zero if there is no pain and these are added together to reach a score between 0 and 19.
The SS measures the severity of the person’s fatigue, sleep quality, cognitive symptoms, and somatic symptoms. Each of these four categories is given a score of 0 – 3 and added together for a total possible score of 12.
Using these new scales, the ACR changed the diagnosis guidelines to:
- WPI ≥ 7 and SS ≥ 5 OR WPI 3–6 and SS ≥ 9
- Symptoms have been persistent for at least three months
- There is no other disorder that could explain the pain
Getting a fibromyalgia diagnosis
Physicians must rely on a patient’s communicated symptoms to make a fibromyalgia diagnosis. Therefore, the first thing a doctor will do is conduct a thorough physical examination of the muscles and joints. After doing this, she or he will then discuss any symptoms a patient is currently having.
Some of main symptoms of fibro include:
- Pain: Constant full body pain with pain at the fibromyalgia tender points
- Unrefreshing sleep: Even after an uninterrupted eight hours
- Fatigue: Chronic fatigue or exhaustion after strenuous activity
- Memory loss: Short-term memory problems coupled with bouts of confusion and inability to concentrate
- Increased pain sensitivity: Hyperalgesia or allodynia
- Depression
Fibromyalgia often is present with other health issues, so a doctor will likely ask about other conditions such as irritable bowel syndrome, headaches, restless leg syndrome, frequent urination, and anxiety.
Since fibro can occur with other illnesses, the next step is to start eliminating more serious medical conditions that could be causing your symptoms. The doctor will run tests on your blood, thyroid, and vitamin D levels. Other tests that could be required are X-rays, computed tomography (CT), and magnetic resonance imaging (MRI). Finally, a biopsy and a physiological exam could be necessary to rule out any suspected mental health issues.
Helping along the diagnosis process
Since fibromyalgia is mainly based off the symptoms that patients share, there are some smart things you can do if you believe you are suffering from fibromyalgia. These tips could save you time, money, and lots of frustration. And, they can help get you back on the path to being healthy and happy faster.
- Make sure to communicate any mental or physical trauma that has occurred to you. A major event like this is sometimes associated with the development of fibro symptoms.
- Keep a pain diary that includes the location of your pain, how it feels, severity, and the length of time it lasts. This can be a perfect tool to parse out fibro from other health issues.
- Choose the right doctor. The stigma around fibromyalgia is fading as more research comes out, but some physicians will be reluctant to diagnose it. Make sure you go to a doctor who is specialized in pain management and has the experience to help you find the right diagnosis.
Finding fibromyalgia treatments
Treatment of fibromyalgia is best approached as a team, with doctors, physical therapists, and other alternative practitioners working together to treat the physical and mental symptoms.
Some treatments include:
- Dietary changes to eliminate anything that causes inflammation or triggers a pain response (e.g., sugar and red meat)
- Changes to exercise plans, including exercises for days when pain is present, and exercise that includes meditation
- Prescription medicines as needed
- Sleep counseling to develop proper sleep habits to combat fatigue
- Changes to work schedules to accommodate good and bad days
Families also play an important role in the treatment of fibromyalgia. Suffering from an “invisible” but chronic illness such as fibromyalgia can be socially isolating. It is important that the family members are supportive of treatment and are understanding when their loved one needs to rest.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) is sponsoring more research on fibromyalgia to better understand this disease, specifically in relation to diagnosis, causes, and better treatments.
To get a fibromyalgia diagnosis, click here to find a certified pain specialist in your area. They have dedicated experience working with fibromyalgia patients and will use the latest diagnostic guidelines to help you diagnose your condition.