Everyone will experience a headache at some point in their life. For those who suffer from migraines, however, the pain can be debilitating. For the 36 million people in the U.S. who suffer from migraines, relief can be hard to come by. Traditional pain relievers typically offer no relief and more potent medications, like opioids, are also powerless against the brutal headaches. Fortunately, researchers have made much headway recently finding new treatment options for migraine patients. Here, we talk about one patient’s journey and then discuss five more potential new migraine treatments on the horizon.
Arizona patient talks about how new migraine treatments helped
For Elizabeth Arant, her migraine pain was constant and had a debilitating impact on her life.
“I’ve had migraines since I was about seven years old. Even as a small child, I would miss school because of the migraines, or from being sick because of the migraines. As an adult, I was worried about work. I would have to excuse myself multiple times a day because I was ill from the constant migraine pain.”
In the beginning, Ms. Arant was treated conservatively with over-the-counter medications, and then eventually, prescription migraine pills and injections.
“I tried all of the migraine medications on the market, and they’d work for a little while, but then they wouldn’t be effective any more. After about ten years, I had tried every migraine medication available.”
When the medications became ineffective, Ms. Arant utilized other new migraine treatments and complementary therapies.
“I tried acupuncture, chiropractic, massage therapy, physical therapy – you name it, I tried it. These treatments would work for a little while, but then the pain would come back.”
Patient turns to interventional pain management options
A diagnostic procedure known as a medial branch block can also be initially tried to see if any relief is achieved. If successful, relief is rapid, and the individual should be able to return to their normal daily activities. While a medial branch block is not intended to cause long-lasting relief, should temporary relief occur from the block, a more permanent form of new migraine treatments called radiofrequency ablation may be recommended by a pain physician.
Radiofrequency ablation (RFA) uses a specialized device to disrupt the nerve that sends pain signals to the brain. By causing nerve destruction through heat, RFA disrupts the perception of pain, effectively causing a decrease in chronic headache pain. More specifically, the sphenopalatine ganglion is a bundle of nerves in the face and head region, and studies have shown success regarding blocks or ablations of those specific nerves.
Ms. Arant tried nerve blocks which, again, helped temporarily, but she was quickly beginning to feel like there was no hope. In Ms. Arant’s case, since conservative treatment was providing only temporary relief, her neurologist referred her to Arizona Pain, where he said a new treatment may be available to her. If conservative treatment such as medication, chiropractic care or non-invasive procedures offer no relief, a device called occipital nerve stimulation (ONS) may prove effective for chronic migraine patients.
Patient tries occipital nerve stimulation
A new use of established technology, ONS works much like a spinal cord stimulator (SCS), commonly known as a “pacemaker for pain.” By utilizing low-level electrical impulses, the ONS replaces pain with a tingling sensation and blocks pain perception from the nerve to the brain.
“Within a few days, I was at Arizona Pain and was being educated by the nurse practitioner and doctor regarding ONS. At that point, I was willing to try anything. I trusted Arizona Pain right away and felt like I really had to try this. Every day, I basically went to work, came home and lay down in a darkened room with ice on my head until I fell asleep. I couldn’t make plans for the future; my quality of life was deteriorating.”
Ms. Arant had the trial stimulator placed, and was surprised at the results.
“In the recovery area at Arizona Pain, I just kept telling everyone that this was the first time in years that I didn’t have a migraine. It was amazing. I was able to read a book, watch TV, and start to get my life back. I knew I wanted to have the permanent device. And, I wanted to keep living without a constant migraine.”
After the initial trial period, Ms. Arant was scheduled to have a permanent ONS implanted.
Patient finds new life
“It did take time to get the settings adjusted,” Ms. Arant says. “But after the settings were adjusted for me, I haven’t had a migraine since. Instead, I have a tingling feeling that is actually pleasant, and not painful at all.”
One word of advice Ms. Arant offers to anyone who suffers from chronic migraines is this:
“If you’ve tried everything else and it’s failed, and your pain doctor is recommending ONS, give it a try.”
The best part is that Ms. Arant is able to do things she hasn’t been able to do in years.
“Now that I have ONS, my life has completely changed. I’m able to travel, make plans, and I’m reading like a maniac. I’m even planning on going to grad school to become a nurse practitioner in neurology to help others that are in constant pain just like I was.”
5 more new migraine treatments
Beyond occipital nerve stimulation, here are five innovative and new migraine treatments available that could help treat your pain.
1. Radiology treatment
A special treatment called intranasal sphenopalatine ganglion is effective enough to reduce the amount of medication migraine patients need to find pain relief, according to research from the Society of Interventional Radiology.
Patients in the study reported a 36% reduction in pain. 88% of study participants said they needed less medication or none at all after receiving the investigational treatment.
The procedure involves administering lidocaine through the nasal passage to the sphenopalatine ganglion. This is a bundle of nerves linked to migraines. Needles do not actually touch the patient during the procedure, making it minimally invasive. Lead researcher Dr. Kenneth Mandato says:
“Administration of lidocaine to the sphenopalatine ganglion acts as a ‘reset button’ for the brain’s migraine circuitry.”
Although the lidocaine ultimately wears off, the procedure seems to deactivate, or at least dampen, the neurological trigger that causes migraines. The procedure is relatively new and untested. However, researchers are hopeful that patients can receive the treatment repeatedly because it’s so minimally invasive.
The treatment isn’t a cure, scientists say, but one more tool in the arsenal against migraine pain. More studies are planned to further quantify the benefits and analyze the long-term benefits of these new migraine treatments.
2. Cosmetic surgery techniques
A technique used in cosmetic eye surgery holds promise for helping migraine sufferers find relief, according to research completed at Louisiana State University Health Sciences Center.
The technique, which involves using an endoscope to travel from the scalp to the eyelid, involves decompressing nerves implicated in triggering migraines. The study found more than 90% of patients felt relief from pain, and slightly more than half of all patients said their migraines completely disappeared. An additional 20% saw an 80% reduction in pain, making this study a huge success story in migraine treatment news.
Not all patients are eligible for the procedure. Factors that would inhibit a patient’s eligibility include individual anatomy, but some doctors aren’t experienced enough with endoscopes to successfully complete the procedure. Study surgeon Dr. Oren Tessler says:
“Although larger studies are needed, we have shown that we can restore these patients to full and productive lives.”
3. Magnet technology
The idea that magnets could potentially be used to treat migraines has been around for decades, but until now, researchers haven’t been able to identify a treatment method using magnetic principles.
In April 2015, Baltimore-based eNerua Inc., announced an infusion of $15 million in capital to release to market a device that soothes migraines by sending magnetic pulses into the brain, reports the Baltimore Sun.
The device, called SpringTMS, works through a coil placed on the scalp from which magnetic waves emanate, similar to a MRI machine. The idea is that the magnetic waves penetrate the skull and travel into the brain where they interfere with electrical impulses contributing to the development of migraines.
The device is convenient in that it can be used at home. To use, patients turn it on with a simple button and place the machine against the backs of their heads when they feel a migraine developing. The treatment lasts less than a minute and offers rapid relief.
The device has already received Food and Drug Administration approval, however it’s only available right now through clinical trials. Monthly treatments cost around $250. The recent influx of capital will pay for additional testing to determine whether the device can prevent headaches instead of just stopping existing ones.
The money will also pay for the product launch, reports the Baltimore Sun. SpringTMS will first be targeted to patients for whom other treatments haven’t worked or who can’t take medication, in case of pregnancy, for example.
4. Social media therapy
It may sound far-fetched, but researchers have found patients experiencing migraines who tweet their feelings experience reduced pain.
University of Michigan researchers analyzed 21,751 tweets from people suffering from a migraine attack and found venting on the social media platform helped them feel better. Researchers say the parts of the brain related to emotion and thinking are also involved in pain perception, which contributed to the decreased feelings of pain.
It may not work, but new migraine treatments are focused on finding any way to prevent or relieve pain.
5. Talk therapy
Talk therapy, also known as cognitive behavioral therapy, is mostly known for its ability to help people resolve emotional pain. It’s not a new practice, but it is one of the most exciting new migraine treatments.
Recent research published in the Journal of the American Medical Association found that it may also be effective for reducing the frequency of chronic migraine episodes in children and adolescents.
The news gave patients hope because there aren’t any approved medications for young people with chronic migraines, limiting treatment options. Patients are considered to have chronic migraines when they have 15 or more migraine episodes each month.
Study participants were divided into two groups. One group received therapy, learning ways to cope with pain in addition to learning biofeedback techniques. The second group participated in a headache education session.
After a year, 86% of patients receiving therapy said the number of migraine days they experienced was cut by at least half. Researchers said the strong data was encouraging, and recommended that cognitive behavioral therapy be offered to young people with chronic migraines as a front-line therapy to complement medicine.
Other research conducted at Ohio University has found that therapy increases the confidence of adult migraine sufferers as they work to self-manage pain. The effect was most dramatic for those who enter therapy without much confidence. This makes therapy an effective way to reach the people who need it most. Science Daily reports:
“Behavioral management also increased participants’ belief that migraines can be influenced by one’s own behavior and decreased the belief that migraines are primarily influenced by chance or fate.”
What new migraine treatments have you found most effective for treating your migraines? Ready to talk to a pain specialist to see how new migraine treatments could help you? Click here to get started.
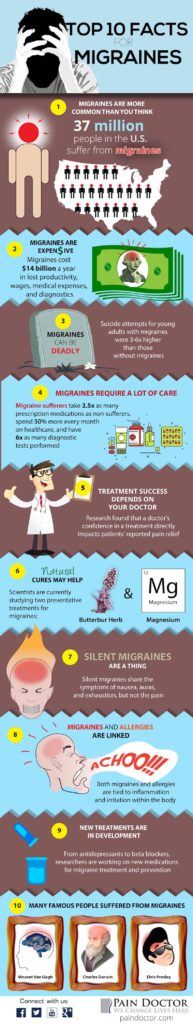
Migraine infographic
Want even more? Check out our infographic that covers the top ten facts about migraines.


Can ONS be used for severe tension headaches and occipital pain??
Hi MaryJean — It depends on the patient. You can find a pain doctor in your area at https://paindoctor.com/find-your-pain-doctor/. They can help you discuss treatment options for tension headache and occipital headache pain.
Mary Jean. Did you pursue the ONS procedure? Where are you located.